Dr. Le Van An has practiced musculoskeletal radiology, as well as general radiology, with the SELARL P.A.R.R.C Medical Group, in Saint-Martin-Boulogne, France, for 17 years. While it is not his area of specialization, reading mammograms is an important part of his practice with the group, which offers both 2D and 3D mammography.
What was your opinion of AI in radiology before you tried MammoScreen™? Were you a sceptic?
I wondered whether artificial intelligence could bring anything to our practice—whether there would be too many false positives and false negatives; whether using it would slow down our workflow and analysis time. We were pleasantly surprised.
When we first started using MammoScreen, we needed to gain confidence in it—see if it had good positive and negative predictive values. It took some time to adapt, but now we trust the software. It’s especially useful for triaging cases.
THE GREEN, THE RED AND THE YELLOW
Mammogram cases are color-coded in three categories: Green, yellow and red. When a mammogram is “green”, we feel confident that it’s negative, so we can accelerate reading time.
There are 2 situations regarding red cases. If it’s a clearly visible lesion we feel more confident in our reading.
Sometimes though, there are little lesions that are more subtle and MammoScreen gives them a red score, which means that there is definitely something abnormal. If I don’t see it using ultrasound, I do an MRI. We’ve been using MammoScreen for a while and have learned that if it marks the case in red, there is really something suspicious, and we have to be cautious.
With calcifications, MammoScreen is a not as dependable. It detects them well but there are sometimes false positives. MammoScreen is too pessimistic in characterizing calcifications.
The most interesting cases are the yellow ones. This is where the radiologist’s expertise and MammoScreen come into play. We might not initially pay much attention, but when MammoScreen displays the yellow score, it means I need to stop right there and double check to see if there is a distortion, or anything abnormal.
Now when I see a yellow case, I systematically take a spot compression view to see if it’s still there. If I have the priors, I compare it to the priors, knowing that some breast cancers are not evolving and remain stable for two years. If the abnormality is visible, I will make an additional ultrasound.
How has using MammoScreen impacted your practice?
Since we started using MammoScreen we are detecting more subtle cancers that we might have missed before. We take more spot compression views and more targeted ultrasound exams that lead to more MRI exams.
I’ve also become very efficient with targeting ultrasounds. I know exactly where we should look, which helps detect lesions of 5-6 millimeters that I might have missed initially.
Sometimes you don’t find anything in ultrasound, which can be annoying.
Given the experience we’ve had with MammoScreen, if the software points at something, I know it is definitely suspicious. If it is still there on a quality spot compression view, but I didn’t see anything in ultrasound, I tend to make an additional complementary MRI. And in a number of cases, that confirms that it is positive.
How long does it take for radiologists to become highly proficient in their work? Do you see AI shortening that learning curve?
In breast imaging it’s very important to train your eyes by seeing many mammograms. Some abnormalities are easily visible, but there are also more subtle ones. You need years and years of practice to learn how to detect them.
This is a problem for young radiologists who haven’t read many mammograms – or even any at all – as students. That’s why they get really stressed when they are asked to read them.
For these radiologists with less experience, I believe MammoScreen is a real safety net. It can help them detect the subtle lesions that would ordinarily require years of practice to identify. This lets them gain proficiency in reading mammograms while feeling confident in their accuracy.
Do you think there is a lot of pressure in the industry to move quickly, read more screens in a day?
We have to increase our productivity and intensify the rhythm in order to cope with cost issues. Another factor is workflow. Examination production time, the time to take the mammogram, the maintenance takes a lot of time.
How big an issue is fatigue for radiologists? How does it affect accuracy? Productivity?
Fatigue is definitely an issue. We are all human. When we’re fresh we are more attentive and more alert in detecting abnormalities. When we get tired, we’re less cautious.
How do you cope with fatigue? Has MammoScreen changed that?
Thanks to MammoScreen, our shifts are less stressful. We know that there is a second reading by the AI, so we feel less anxious. A green mammogram is reassuring. MammoScreen also allows us to be more confident about subtle abnormalities because the software confirms what we have detected.
Talk about a few of your cases where MammoScreen made a difference.
There was a case with a lesion with density that was already present on the prior. We thought it was stable, but since MammoScreen pointed it out, we made a targeted ultrasound. (SEE CASE 1)
In another case, the lesion was not clearly visible at first glance. But when we made spot compression views, we found some suspicious lesions, confirmed by biopsy. MammoScreen can be helpful with these subtle lesions. (SEE CASE 2)
Sometimes we get this feeling of accomplishment when we find a cancer. We’re so proud of ourselves that we may not look attentively enough at other lesions. We shouldn’t be so biased by our professional satisfaction that we don’t look for the second cancer. MammoScreen helps us to watch the other lesions.
What would you tell radiologists who haven’t tried MammoScreen?
I would highly recommend trying MammoScreen, it reduces your stress at work, lets you feel less anxious and more confident. Moreover, it’s beneficial for the patients as well, since it helps catch cancers.
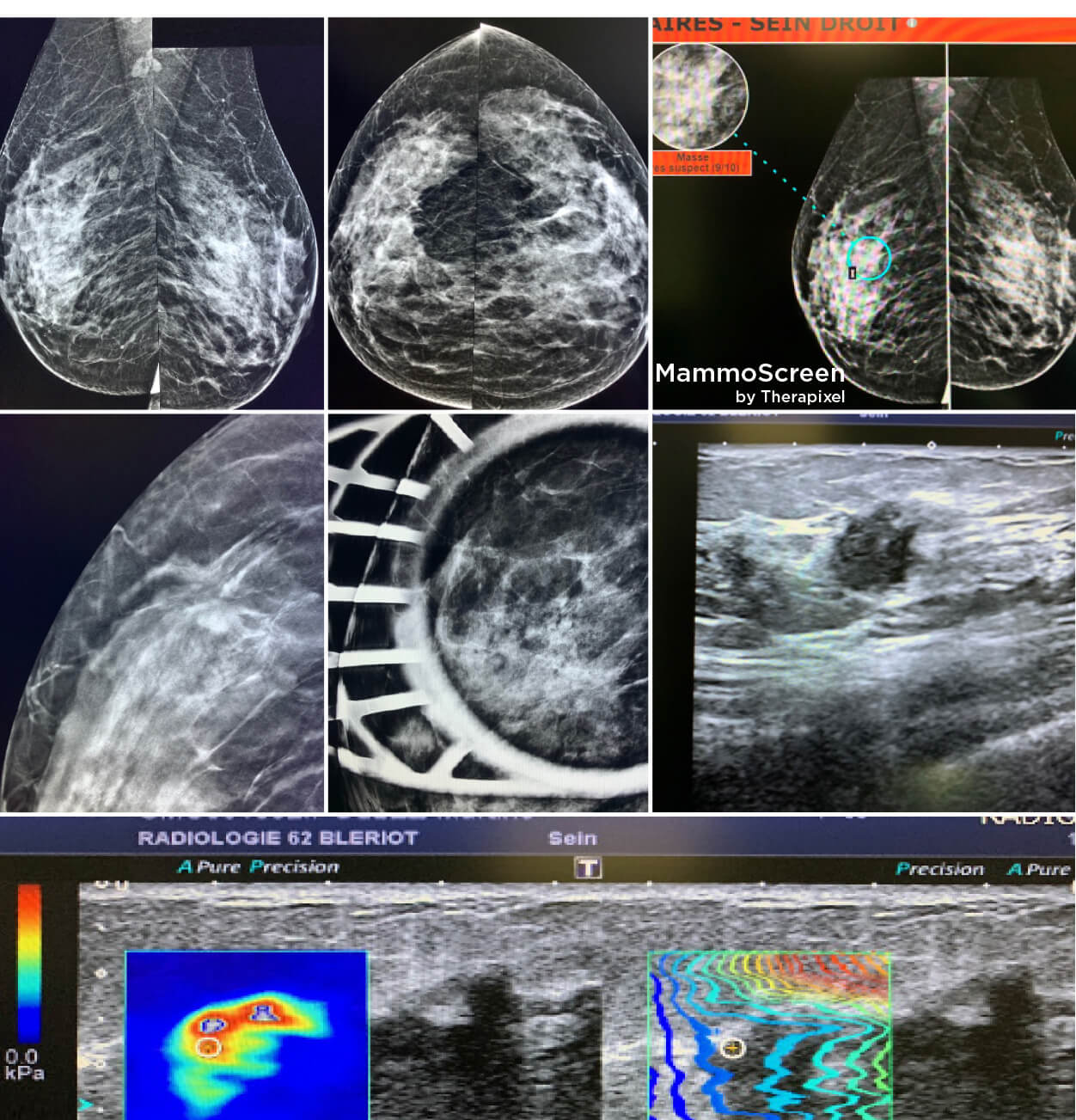
CASE 1
A 73-y.o. woman, breast screening. 2 years before her screening mammogram was considered normal by two readers.
At first glance, the new breast mammogram was also considered normal and unchanged compared to the prior, but MammoScreen™ by Therapixel pointed out at a lesion of the right breast. The retrospective analysis of the prior by MammoScreen pointed at the same area.
MRI demonstrated a spiculated mass of the right breast. At first look, my colleague didn’t succeed to find the lesion in echography and unsuccessfully tried macro biopsy twice.
Finally, another colleague succeeded to locate it by echography and made an ultrasound-guided microbiopsy: invasive breast carcinoma luminal A type.
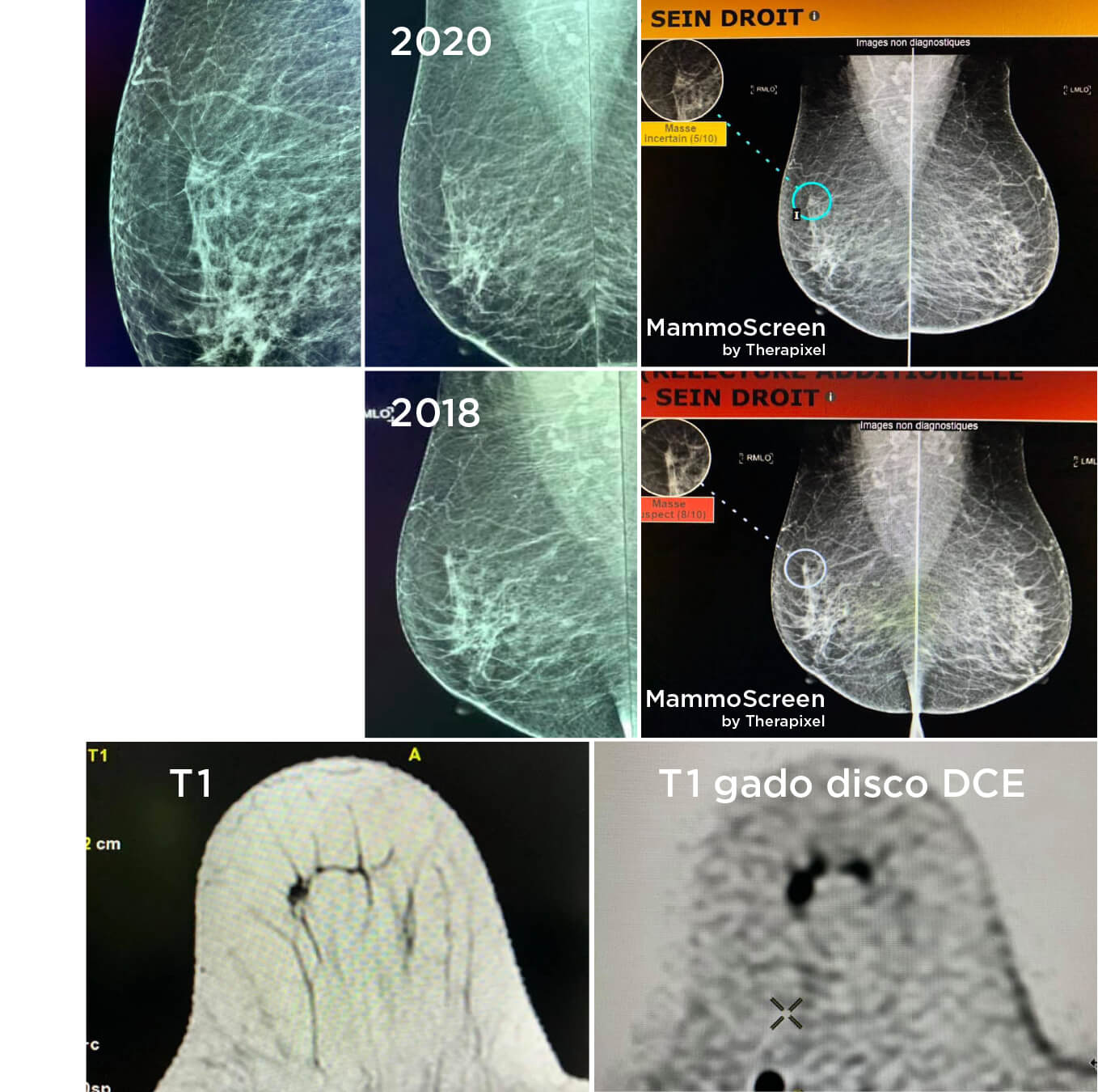
CASE 2
Woman, 50 y.o., screening mammography.
At first glance, the mammogram seemed normal. Tomosynthesis showed a possible distortion, but between a crossing of fibers and a not very easy pathological image. MammoScreen™ pointed out an external retromammelonal zone. I made the front and profile spot compression views but that did not bring out a spiculated image. As MammoScreen highlighted the case in red, I thought that as a precaution I should persist.
Therefore, I made an ultrasound scan that highlighted a hypoechogenic image with irregular contours, with zones of rigidity under elastographic study, located at the union of the external quadrants of the left breast. Ultrasound shows a hypoechoic mass with irregular contours and elastographic rigidity.
BREAST BIOPSY: INFILTRATING CARCINOMA OF LUMINAL HER2+ TYPE